Evidence Base Guidelines, Recent Research on Acupuncture for Endometriosis, and the Accredited Register of Acupuncturists in the Healthcare Sector.
Holly:
“To be told by a healthcare professional that potentially I may require donor eggs for IVF, due to my stage 4 endometriosis, was a shock. That was not the case, and our first son is finally here. We cherish every moment with our son. We cannot believe we got to see him at only one cell in a petri dish. IVF/ICSI is just incredible. We feel fortunate it worked for us. I am certain this first round of medical treatment was significantly increased by the acupuncture sessions I attended before IVF for my endometriosis and painful cycles. Lianne helped put me at ease during one of the most stressful times of my life and for that I am very thankful. If you are considering whether acupuncture is worth it, and how it can help, my advice to you is give it a go; you will not regret it.”
Endometriosis
What is Endometriosis?
Endometriosis is a chronic inflammatory condition defined by the occurrence of endometrial-like tissue outside the uterus. This endometrial type of tissue grows in different parts of the body. During the menstrual cycle, these cells mimic the endometrial cells of the womb lining by building up and breaking down. This results in bleeding outside the womb in parts of the body and places where no bleeding should occur. Unfortunately, this results in pain, inflammation, and scar tissue. 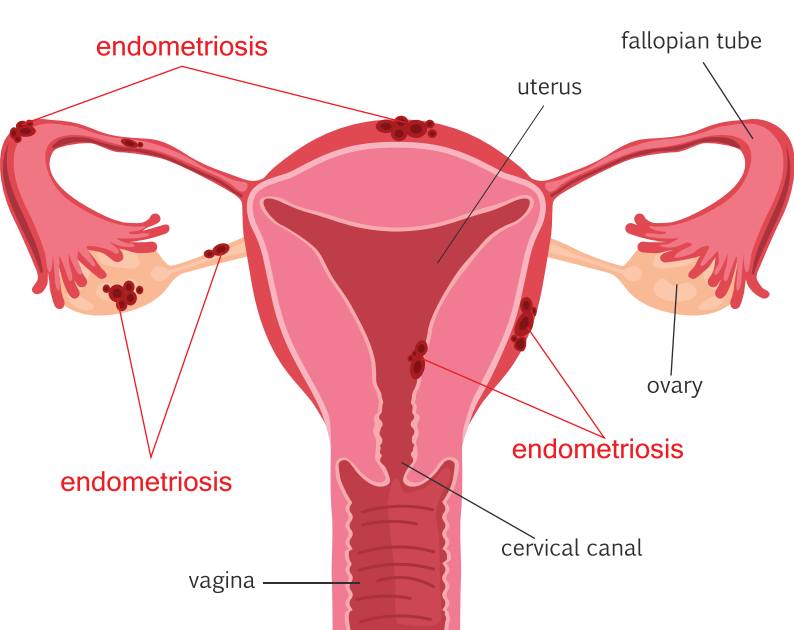
Endometriosis is classified as hormone related. The exact cause of endometriosis remains unknown. What is known is that endometriosis affects an estimated 190 million females globally, and approximately 1.5 million females here in the UK.
Impact of Endometriosis
Endometriosis can cause severe pelvic pain, period pain, heavy bleeding, and pain during and after sexual intercourse. Pain can occur during a bowel movement, and urination. There may be rectal bleeding or blood in urine. Women can experience abdominal bloating, and fatigue. Endometriosis can also lead to fertility problems. Other symptoms suggestive of endometriosis include cyclical cough, chest pain, shoulder tip pain, and catamenial pneumothorax. It is important to note that this chronic condition can seriously affect a woman’s quality of life, including their physical, psychological, emotional health and wellbeing.
Diagnosis of Endometriosis
The diagnostic outcomes and symptoms can vary between investigations and individuals. Due to this complexity, the diagnosis of endometriosis has been described as problematic. The estimated time delay from the onset of the symptoms of endometriosis to a diagnosis of endometriosis averages eight years. Awareness of the condition, clinical examination, and imaging (ultrasound or MRI) can aid endometriosis diagnosis. Where relevant, particularly in the case of a negative diagnostic finding for endometriosis via imaging, or when empirical treatment for endometriosis is unsuccessful, the offering of a laparoscopy for diagnosis and treatment management is advised.1 A vital question to ask is: what are the treatment options for women suffering from endometriosis? Although there is currently no cure for endometriosis, treatments are offered with the aim of easing the debilitating symptoms. The European Society of Reproductive Medicine (ESHRE) highlight that treatments for endometriosis can offer partial or temporary pain relief, and that symptoms often reoccur after discontinuation of treatment.
Treatment Options
The treatment management of endometriosis outlined by National Health Service includes over the counter painkillers, the prescribing of medication, hormone therapy, and surgery.2 The ESHRE update for treatment management of endometriosis states that there are limitation reasons for caution around the evidence base for this condition, and that therefore, no firm recommendations could be made on the most appropriate treatment.3
Pain Management
It should be noted that there are weak or strong healthcare recommendations for the management of endometriosis associated pain based on the limited evidence base. For example, a weak recommendation for the use of analgesics (paracetamol and non-steroidal anti- inflammatories) based on “very low-quality” evidence. Or a strong recommendation for surgery to reduce endometriosis associated pain based on limited evidence. In addition, ESHRE describes that medications such as amitriptyline, nortriptyline, duloxetine, gabapentine and pregabalin have shown promise in the treatment of pain resulting from endometriosis, yet these pharmaceuticals have not been proven to be superior to placebo and can have severe, dose-limiting side effects. Recently, a systematic review and metanalysis published on acupuncture for endometriosis found that acupuncture was beneficial for pelvic pain and menstrual pain. The quality of the evidence is considered low. However, in the grand scheme of the available quality of evidence base on which treatment options and recommendations are made, acupuncture in a research output is more than a promising intervention.4 Acupuncture treatment for endometriosis demonstrated clinically relevant improvements in pelvic pain. More about this later…
Hormone Treatments
ESHRE strongly recommend hormone treatments for endometriosis-associated pain, including combined hormonal treatment, progestogens, GnRH agonists or GnRH antagonists. The efficacy of combined hormonal treatments is believed to have been summarised and justified within systematic reviews according to guidelines and these are outlined below. A systematic review on “hormonal contraception in women with endometriosis” incorporated for the care of women with endometriosis was interpreted as: oral contraceptive pills result in statistically significant reduced endometriosis-related pain, resulting in improvement in quality of life. The systematic review, however, omits an essential requirement, which is to assess and adequately report on the risk of bias. Amazingly, the authors “skirt” around the key issue by inserting the statement: “the quality of studies was not always high.” Just how did this systematic review (that declares using a PRIMSA tool) get through a peer review process, publication, and still not adequately nor appropriately present the risk of bias in the studies? The authors of this review do mention a sentence in the limitation section and you would need a magnifying glass “… the results of this systematic review must be considered with caution and expanded in future studies”.5 Another recommendation was justified based on the positive findings that resulted from a systematic review of combined hormonal contraceptives for the treatment of endometriosis-related pain. Findings were advocated due to clinically important and statistically significant reductions in endometriosis-related pain. The researchers who conducted this study, in fact, conclude that the supportive data are of low quality.6 Further, similar incidents occurred. A different systematic review was applied to justify a recommendation of hormonal contraceptives. It was highlighted that oral hormonal contraceptives were shown to be associated with clinical improvements. The truth, however – according to the authors who conducted the study – is that the evidence base and findings are classified at a high risk of bias. The quality of evidence available was classified as “very low-quality” evidence. Another really disturbing finding that was completely missed by the reviewers compiling the guideline, is the part where the authors of this research announce that: “There appeared to have been substantial involvement of the pharmaceutical company funding the trials.” 7
Progestogens and anti-progestogens
The guideline presents a Cochrane review that is stated to have found both continuous progestogens and continuous gestrinone are effective therapies for the treatment of endometriosis associated pain. This is incorrect. The authors of this review clearly conclude that there is only limited evidence to support the use of progestogens and anti-progestogens for pain associated with endometriosis.8 “Main results The progestagen medroxyprogesterone acetate (100 mg daily) appeared to be more effective at reducing all symptoms up to 12 months of follow‐up compared with placebo. There was evidence of significantly more cases of acne (six versus one) and oedema (11 versus one) in the medroxyprogesterone acetate group compared with placebo. There was no evidence of a difference in objective efficacy between dydrogesterone and placebo. There was no evidence of a benefit with depot administration of progestagens versus other treatments (low dose oral contraceptive or leuprolide acetate) for reduced symptoms. The depot progestagen group experienced significantly more adverse effects. There was no overall evidence of a benefit of oral progestagens over other medical treatment at six months of follow‐up for self‐reported efficacy. Amenorrhoea and bleeding were more frequently reported in the progestagen group compared with other treatment groups. There was no evidence of a benefit of anti‐progestagens (gestrinone) compared with danazol.” Authors’ conclusions There is only limited evidence to support the use of progestagens and anti‐progestagens for pain associated with endometriosis.” It is acknowledged in the guideline that conclusions must be treated with caution due to the paucity of data. Conversely, there is a strong recommendation to prescribe women progestogens to reduce endometriosis pain. Guidance does indicate to take account the different side effect profiles. The team concludes that despite all these issues there is “sufficient” evidence for progestogens and anti- progestrones. The evidence for hormonal treatments links back to 2017 and is based on the National Institute for Health and Care Excellence (NICE) guideline [NG73] Endometriosis: diagnosis and management.9 A network meta-analysis (NMA) was conducted of hormone treatment for pain relief and the visual analogue scale. This NMA is considered to quite conclusively show that all of the hormone treatments work for pain relief on the visual analogue scale compared to placebo. In the report it states that rarely were details of randomisation or allocation concealment reported in the trials.
Gonadotrophin-releasing hormone analogues for endometriosis (GnRHas)
An updated version, however, on gonadotrophin-releasing hormones for endometriosis published in 2023 found that, for overall pain, there might be a light decrease in favour of treatment with GnRHas when compared to placebo, oral or injectable progestogens. However, due to “very low” or “low certainty” evidence, the results should be interpreted with caution. The main limitations presented by the researchers were that all the studies suffered from serious risk of bias due to poor reporting of study methods, and serious imprecision.10 There is a recommendation for GnRHas.
Surgical Treatment for Endometriosis
 Surgery is recommended as an option to reduce endometriosis-associated pain. The guideline does discuss that there is uncertainty regarding the effect of laparoscopy and laparoscopic intervention, which limited any valid conclusion on the benefit of surgery for the treatment of pain. A central review applied to aid decision-making for surgery consisted of before and after studies (of varied study design). The review explored the effect of surgical intervention on pain and quality of life. The authors of the study state that they found that surgical treatment for all types of endometriosis, deep infiltrative endometriosis (DIE), and bowel endometriosis resulted in improvement in major domains of HRQOL, with emphasis on bodily pain. The authors confirm that they assessed the risk of bias using relevant assessment tools: “The Quality Assessment of Controlled Intervention Studies and the Quality Assessment Tool for Before and After Studies with No Control.” 11 Of the studies rated, only 8 studies were assessed as good, leaving 31 remaining studies that had around 50% of the required criteria unfulfilled. 12 For more information the ESHRE Guideline for Endometriosis 2022 can be accessed here. The National Institute of Clinical Excellence (NICE) is updating the Endometriosis: diagnosis and management guideline and should include the new research of acupuncture in the process. The Endometriosis: diagnosis and management NICE guideline [NG73] Published: 2017 can be accessed here. As mentioned, the cause of endometriosis is unknown, but here are several associated theories, including genetics, a person’s immune system and inflammatory processes. However, none of those theories are thought to fully explain why endometriosis happens.
Surgery is recommended as an option to reduce endometriosis-associated pain. The guideline does discuss that there is uncertainty regarding the effect of laparoscopy and laparoscopic intervention, which limited any valid conclusion on the benefit of surgery for the treatment of pain. A central review applied to aid decision-making for surgery consisted of before and after studies (of varied study design). The review explored the effect of surgical intervention on pain and quality of life. The authors of the study state that they found that surgical treatment for all types of endometriosis, deep infiltrative endometriosis (DIE), and bowel endometriosis resulted in improvement in major domains of HRQOL, with emphasis on bodily pain. The authors confirm that they assessed the risk of bias using relevant assessment tools: “The Quality Assessment of Controlled Intervention Studies and the Quality Assessment Tool for Before and After Studies with No Control.” 11 Of the studies rated, only 8 studies were assessed as good, leaving 31 remaining studies that had around 50% of the required criteria unfulfilled. 12 For more information the ESHRE Guideline for Endometriosis 2022 can be accessed here. The National Institute of Clinical Excellence (NICE) is updating the Endometriosis: diagnosis and management guideline and should include the new research of acupuncture in the process. The Endometriosis: diagnosis and management NICE guideline [NG73] Published: 2017 can be accessed here. As mentioned, the cause of endometriosis is unknown, but here are several associated theories, including genetics, a person’s immune system and inflammatory processes. However, none of those theories are thought to fully explain why endometriosis happens.
Acupuncture
Traditional Acupuncture
On the topic of theory, an acupuncturist’s perspective of endometriosis also includes complexity, albeit manageable complexity. The diagnosis and treatment strategy are based on the collection and differentiation of the presenting symptoms of an individual. This also includes their psychological and emotional context. Patterns of disease can generally be subclassified as Endometriosis due to Blood-Stasis and Qi Stagnation; Endometriosis due to Cold-Stasis; Endometriosis due to Blood-Stasis and Heat; Damp-Heat; and/or Kidney Deficiency. These pathophysiological mechanisms are associated with the quality, consistency, and flow of “blood”. To Provide some detail, severe stabbing pain that is worse when applying pressure, accompanied by abdominal bloating, and represented by specific correlating clinical findings (e.g. a purple coloured tongue body) would be classified by the clinician as a “Blood-stasis” pattern and the acupuncture treatment strategy modified accordingly. Whereas pain that is dull, mild, and relieved by applying pressure and warmth could be classified as a kidney deficiency pattern and so on. 13 It is important to highlight that classification may consist of multivariate patterns. Also, conditions are not limited to the patterning outlined above. Complexity of the condition may require a range of strategies, varied dose, and duration based on an individual’s case history. For these reasons, it is necessary to find a qualified acupuncturist with a specialist qualification (degree level or higher) from an educational establishment that obtained the British Acupuncture Accreditation Board (BAAB) quality mark. To find out more about the BAAB click here.
Acupuncture and Moxibustion for Endometriosis: A Systematic Review
A systematic review of acupuncture found insufficient evidence on the overall effectiveness of acupuncture and moxibustion for endometriosis. The researchers found that their research was limited to single studies of low to moderate certainty. The studies showed acupuncture may improve endometriosis pain-related symptoms and improve quality of life, with few adverse events presenting. Acupuncture plus conventional therapy indicated greater improvements for patients. However, more research is most certainly required to explore this finding. 14
Acupuncture for Endometriosis: Systematic Review and Meta-analysis
Recently 2023 a group of scientists explored the effects of acupuncture for endometriosis and found low-quality evidence for the positive impact of acupuncture for endometriosis. Low-quality evidence means that you cannot be certain of the positive effects that were found to have occurred. The researchers concluded as a result of their scientific investigation that acupuncture had positive effects and beneficial outcomes for females suffering from endometriosis-associated pelvic pain (low certainty) and menstrual pain (moderate certainty), and that acupuncture should be considered as a potential treatment intervention.15 “Evidence of effectiveness was found for acupuncture for pelvic pain, and menstrual pain.” “Acupuncture should be considered in the clinical management of endometriosis for those who have not responded to other interventions and where pelvic pain is a primary concern.” The authors conclude that acupuncture may cause a large reduction in pelvic pain compared to non-specific acupuncture at the end of treatment. It is reported as uncertain whether this reduction in pain continues after cessation of treatment as studies did not report this. To note, most studies recounted low rates of adverse events. Charlotte suffered endometriosis and shares her treatment management journey: “I was diagnosed with endometriosis over seven years ago, after coming off birth control to find myself experiencing unbearable periods. Pain, migraines, and crippling anxiety were occurring cyclically for me. Eventually, I found Chinese medicine, which has made a significant difference. Through acupuncture, herbs, bio-identical progesterone and lifestyle changes, my endometriosis is comfortably controlled, and a recent MRI shows that the lesions have slightly improved. I now advocate for body autonomy and informed choice within medicine.” Charlotte Keech
Acupuncture and Endometriosis
What I recommend, when it comes to best practice and the care of women with endometriosis for the partial or temporary relief of painful symptoms, is to try acupuncture. Treatment options are commonly in the clinical setting, tested for efficacy, and when ineffective require trying a range of alternative approaches to ascertain what works and does not work for an individual. Acupuncture is no different. You may not be aware that acupuncture is a treatment option, particularly as it is not included in guidelines, and sources wrongly state there is no evidence supporting acupuncture as a treatment. It will become evident whether an acupuncturist is helping to manage endometriosis-associated pain and a person’s quality of life improves. Feedback, visual analogue pain scales, other validated tools can be incorporated to monitor pain reduction within teams. A primary or secondary healthcare provider can refer direct to an acupuncturist on an accredited register for health and social care. Patients can also self-refer at the British Acupuncture Council: Find Us To find a qualified herbalist visit the Register of Chinese Herbal Medicine: Find Us
Summary
Treatment should consider a range of options, the actual evidence bases’ status, offer a choice, be in line with patient preference and circumstance, consider the side effects and cost, and not be biased towards excluding the role of integrated treatments such as acupuncture and acupuncturists as part of a multidisciplinary network team. I would like to draw attention to acupuncture as a treatment option. There is absolutely no reason why acupuncture should not be offered within integrated patient pathways. An estimated 1.6 million women in the UK are affected by endometriosis. There is a need for funding of research, and a range of new study methodologies designed toward high-quality outputs, innovative treatments to improve the quality and efficacy of the treatment options for pain management, and prevention of disease escalation and complications.
Lianne Aquilina RDN, BSc Hons, MBAcC, MSc
Lianne is an individual expert for draft healthcare guidelines, consults on evidence base policy development for registered health professions. She is a peer reviewer of research prior to publication. Lianne’s current research project is exploring the clinical practice of Chinese herbal medicine for threatened miscarriage at inpatient and outpatient hospital settings in China. Lianne is a member of the British Acupuncture Council. The Professional Standards authority protects the public by overseeing the regulation and registration of healthcare professionals. The PSA oversees registrant members of the British Acupuncture Council.
Resources
Endometriosis UK Pain and Symptom Diary Endometriosis Get Support
Want to know more? Read how acupuncture helped Sindu below:
Sindu
“My husband and I had been trying to conceive for about a year after a range of blood tests, ultrasounds and laparoscopic surgery, I was diagnosed with endometriosis and had a 7cm endometrioma removed from my left ovary. I had IVF and it failed. We were devastated. For our next IVF cycle, I decided to try acupuncture to help me prepare both physically, and emotionally. My acupuncturist supported us through this time with information and research so that we could make the most informed decisions we could. I also continued my acupuncture treatment during ovarian stimulation and embryo transfer to ensure the most hospitable environment possible. I experienced a healthy, normal, and low-risk pregnancy. I am absolutely convinced of the importance of acupuncture in our fertility journey and will definitely return in the future. Our baby girl arrived at home, and we are thankful that we are all doing well. We thank our acupuncturist so much for the role she played in bringing her into the world.”

Lianne Aquilina RDN, Dip Ay, BSc Hons, MSc, PGDip, MBAcC, MATCM, MAAC, MBMAS, MRCHM
Director of Aquilia Acupuncture
Acupuncturist, Researcher
This is an opinion piece outlining a new cohort study in press that examined the link between acupuncture during ovarian hyperstimulation and live birth rates.
Lianne holds a specialised Master of Science in Applied Health Research from the University of York. She has over twenty years of experience as an acupuncturist and has served as a visiting guest lecturer on acupuncture for IVF and the critical appraisal of research. Lianne is a trustee of the Research Council for Complementary Medicine UK. She contributed to the European Society of Human Reproduction and Embryology (ESHRE) guidelines on the number of embryos to transfer during IVF/ICSI. She is an independent UK expert in research. She is coauthor of the best-selling international textbook for acupuncturists, “Acupuncture for IVF: An Integrated Approach to Treatment Management.”















